The real-world use of Artificial Intelligence (AI) in healthcare inspires us to adopt AI methodologies actively. The aim is to create a transformative paradigm for the healthcare and medical sectors by leveraging emerging technologies.
Many researchers place considerable emphasis on how AI can streamline healthcare operations. For instance, AI-driven tools enhance diagnostic accuracy and prognosis, serving as significant aids in care planning.
The notable advantages of AI have led scientists to believe that it can become an essential component of healthcare services in the near future, offering vital functionalities across various clinical areas.
This belief has spurred both technology companies and government entities to develop AI tools and invest in medical applications. As a result, patients stand to benefit from innovative AI-based solutions, being among the first to experience these advancements. Moreover, how patients perceive these tools can significantly influence their integration into clinical care.
However, it’s crucial to ensure that AI-based tools are safe for patients. Before implementing such advanced technologies in direct patient care, all associated risks and concerns must be thoroughly addressed.
This leads to an essential question: How can an artificial tool effectively imitate human capabilities and offer assistance? The technology behind these advancements is truly extraordinary.
AI tools are designed to replicate human cognitive functions, supported by vast amounts of clinical data and rapid advancements in analytical techniques.
With numerous potential applications, AI can integrate into healthcare in various ways. Common methods include machine learning techniques for structured data, such as Neural Networks and deep learning, as well as unstructured data processing.
**Impact of AI in the Healthcare Sector:**
AI can employ sophisticated algorithms to extract insights from healthcare data, thereby supporting clinical care. Furthermore, these tools can help minimize inevitable human errors in therapy and diagnosis.
Additionally, AI can gather valuable insights from expansive patient populations to inform risk assessments or predict health outcomes. However, before these AI systems can be integrated into clinical applications, they need to be trained on previously collected medical data.
Through this training process, the tools learn to recognize and understand patterns across similar patient groups. Major data sources include comprehensive physical examination records and clinical laboratory results, which can be converted into analyzable text. This allows AI to process the information and create understandable electronic medical records (EMRs) for further evaluation.
But what about the devices? In medical applications, AI devices typically fall into two categories: machine learning-based analysis of structured data like imaging and natural language processing (NLP) techniques that extract information from unstructured data, such as medical notes.
Interestingly, the cognitive ecosystem that these unique tools represent, paired with predictive and corrective architectures, can effectively emulate human-like thought processes on computers.
Despite the extensive literature on AI in healthcare, research has often concentrated on a limited number of diseases, particularly cancer, neurological disorders, and cardiovascular issues. However, as technology evolves, so do the tools, leading to increased research across a broader range of diseases.
Among these advancements, Simbo stands out as a groundbreaking upgrade in healthcare, showcasing its ability to mimic human behavior and meet the demands of clinical operations.
**Final Thoughts:**
The AI-powered tools behind Simbo are exceptionally equipped to assist doctors in their daily tasks, enhancing patient care significantly.
With a voice-activated doctor assistant and a digital helper, Simbo provides real-time support to patients requiring immediate attention, embodying human-like thought processes. Embrace Simbo to experience the future of healthcare.
The Future of Medical Transcription in the Age of Voice Technology: What Lies Ahead in 2023
Automatic speech recognition (ASR) technology, powered by artificial neural networks, is slowly transforming the medical industry.
Doctors are increasingly prioritizing patient care over monotonous administrative tasks, and a significant reason for this shift is the rise of artificial intelligence (AI). Artificial neural networks (ANN) are enhancing various sectors, including data science, medicine, and translation. In this article, we will explore how AI and translation technologies are shaping medical transcription, highlighting the synergy between data science, healthcare, and linguistic services for the greater good. We will focus on the influence of ANN on the medical sector, particularly the challenges posed by ASR and the language barriers it may create in doctor-patient communications.
Understanding Medical Transcription
Medical transcription is a practice that has been around for many years, gaining prominence with the advent of electronic health record systems in the 1960s. Before medical transcription became standard, healthcare professionals manually documented their patients’ health conditions and tracked their follow-up visits.
This manual transcription process was often time-consuming, which in turn delayed patient treatment. Consequently, the idea of hiring or outsourcing medical transcription services gained traction. But what exactly does medical transcription entail? How does it operate? This article will provide a comprehensive overview of medical transcription.
Medical transcription (MT) refers to the procedure of converting voice-recorded medical reports—dictated by physicians and other healthcare providers—into written text. These voice reports can encompass clinical summaries, lab results, surgical notes, and other health-related documentation. The primary purpose of medical transcription is to establish a written record of a patient’s medical history, which can be either printed and retained as physical documents or saved electronically.
Emerging Trends in Medical Transcription
The medical field is constantly evolving, with new and innovative technologies reshaping practices and enhancing patient care and safety. Advances in medical transcription are a clear indication of this ongoing transformation. This process not only involves converting physician dictation into text but also integrating the resulting documentation into electronic health records (EHR). Additionally, it includes editing and proofreading reports generated by voice recognition systems.
Medical transcriptionists possess a deep understanding of medical terminology and jargon. They meticulously check for accuracy in punctuation, grammar, and language, utilizing word processing software to ensure that precise records are generated. As a result, many healthcare providers are outsourcing medical transcription to maintain the accuracy of EHR documentation.
- Voice Recognition Software:
Voice recognition software is becoming increasingly popular among medical practices, helping to streamline workflows. Given the fast-paced nature of modern healthcare environments, many physicians favor hands-free dictation over traditional typing. The advanced features of this technology enable them to concentrate more on patient interactions rather than splitting their focus with computer typing during consultations.
- Advanced Reporting Techniques:
Traditional recording devices are being largely replaced by advanced reporting tools and services. The use of electronic consoles, word processors, and devices equipped with integrated voice recognition and memory storage capabilities is significantly increasing the demand for recording service providers.
- New Medical Documentation Formats:
The medical transcription industry is moving away from simple word-processed documents to comply with EHR standards. The new formats incorporate point-and-click fields, drop-down menus, and structured templates, leading to a more systematic approach to documenting patient data.
- Secure Networks:
Mobile medical transcription is now a reality, enabling the use of smartphones or tablets for this purpose. Enhanced network security ensures that shared data remains protected.
The Transformational Role of Voice Technology in Healthcare for 2023
Voice technology offers the most natural way to communicate, enabling individuals to convey their thoughts and needs effortlessly. In the past, the primary interaction involved typing keywords into a computer or mobile device to access information.
However, with recent breakthroughs in voice recognition, obtaining information no longer requires you to be in front of a screen. Technology has advanced to a point where simply speaking can instruct machines to respond, making the interaction more seamless.
Voice technology is set to revolutionize the healthcare sector due to its intuitive interface and growing acceptance among users. Let’s explore the various applications where notable medical organizations are embracing this exciting wave of voice technology.
We’re witnessing a surge in adoption from both patients and healthcare systems. As more individuals find voice-activated devices like Microsoft’s Cortana, Amazon’s Alexa, and Google Home more accessible, many hospitals are developing voice-activated tools for patient use. The positive response from users confirms the success of these efforts.
On the technological front, developers are diligently enhancing the quality of voice recognition software. Innovative solutions aimed at helping patients manage both acute and chronic medical conditions are also under development.
This advancement is beneficial for patients, healthcare providers, and tech experts alike. The ongoing improvements in speech recognition technology, combined with decreasing device costs, present exciting prospects for medical organizations. As voice technology evolves, patients will find it simpler to manage their health from the comfort of home through voice-assisted Internet of Things (IoT) applications.
Technological Tools in Medical Transcription
Here are some of the common technologies and equipment utilized in the medical transcription industry:
- Digital microphones.
- Transcription software for PCs.
- Digital transcription stations.
- Software for fast typing.
- Telephone dictation software.
- Dictation management software.
- Reference guides for transcriptionists.
- Medical spellcheckers.
- Microcassette voice recorders.
- Fingerless transcription gloves.
- Failure To Progress (FTP) client software.
- Encryption software for audio files.
- Meeting recorders.
- Universal foot pedals.
- Stedman’s electronic medical dictionary.
- Phone dictation solutions.
In Conclusion: The Future of Medical Transcription
As the older population continues to grow, there will be an increased need for medical visits and report generation. The demand for medical transcription is poised to rise along with patient needs, ensuring its vital role within the healthcare landscape.
What is a Hierarchy in Healthcare?
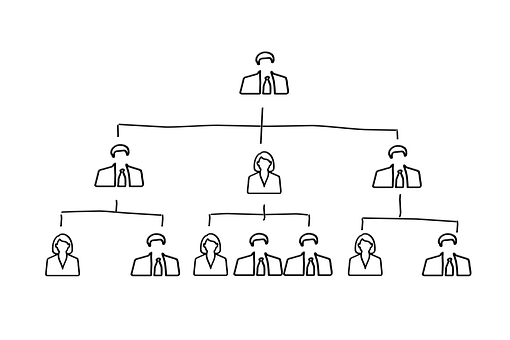
Most healthcare organizations today, including the National Health Service (NHS), operate under a hierarchical, pyramidal leadership model. This type of leadership is characterized by a “clearly defined chain of command that extends from the lower to the upper levels of an organization.”
Structure of Hierarchy in Healthcare
Typically, larger organizations possess a hierarchical structure based on various levels of authority, forming a chain of command that interlinks multiple management tiers within the organization. Decisions are usually made in a formal, top-down manner.
What is the Hospital Hierarchy?
The hierarchy within hospitals can differ by location, but it generally features a general manager and medical directors at the top, with medical assistants at the bottom.
Here’s an overview of the typical hospital hierarchy, starting from senior positions to lower-level roles:
- Manager in Charge:
This top-level official oversees the hospital’s administration, responsible for crafting and implementing policies that ensure patient safety and promote recovery. They also manage the hospital’s financial health regarding budgets and the operational viability of different departments.
- Medical Executives:
Larger hospitals often have multiple medical directors, while smaller ones might only have one or two. These directors are tasked with formulating safe and effective healthcare policies and should always be aiming to uphold high standards of patient care. They oversee nearly all aspects of both inpatient and outpatient services, with some managing specific teams of specialists while others provide more general oversight. Every physician in the hospital reports to a medical director.
- Department Head:
Department heads are specialized doctors leading fields such as orthopaedics, oncology, and pediatrics. In a hospital setting, they create and coordinate medical strategies, guiding attending physicians who follow their direction. Should an attending physician be unavailable due to emergencies, department heads may step in to assist.
- Attending Physician:
Attending physicians are senior doctors responsible for overseeing patient treatment plans. They must possess a minimum of three years of residency experience, with many working in specialized areas.
- Nurse Practitioner:
Nurse practitioners typically interact with patients directly, providing urgent, primary, and specialized care to specific populations, including children, women, and the elderly. Their duties include documenting medical histories, collecting patient samples, ordering lab tests, and performing a variety of direct patient care tasks.
- Pharmacist in a Hospital:
Pharmacists dispense prescription medications and guide patients in their safe use. They may also conduct health screenings, administer vaccines, and oversee medication management in the hospital.
- Specialist in Clinical Nursing:
Clinical nurse specialists can order tests, make diagnoses, provide basic treatments, and in certain states, prescribe medications within a hospital. They also offer expertise and support to the nursing staff.
- Nurse Technician:
Nurse technicians receive additional medical training beyond standard nursing, allowing them to undertake more technical tasks such as inserting catheters, removing stitches, and operating advanced monitoring equipment.
- Registered Nurse:
In a hospital, registered nurses (RNs) handle a broad array of responsibilities, including prepping patients for exams and treatments, administering medications, and educating patients and their families about care processes.
- Assisting in the Medical Field:
Medical assistants represent one of the entry-level positions in hospitals, engaged in various administrative tasks. They may schedule patient appointments, follow up on care, and assist with bookkeeping and billing, most of their work taking place at a desk.
Why is Hierarchy Beneficial in Healthcare?
The fundamental purpose of hierarchy is to help us navigate the complexities of the world, simplify information, and facilitate decision-making. Think of it evolutionarily: when someone declared, “Throw the spear now to take down the mammoth,” their leadership was vital.
A well-established hierarchy holds leaders accountable for outcomes and sets up mechanisms for replacing ineffective leaders, sometimes through promotions from within. This structure ultimately contributes to the success of the organization as a whole, encompassing owners, managers, and employees alike.
What is the Purpose of Hierarchy in Healthcare?
As employees ascend the hierarchical structure, their level of authority increases. Authority is essential whenever leadership is necessary, ensuring that those under a manager work collectively towards the organizational goals—or face potential consequences.
Understanding the Difference Between Machine Learning (ML) and Artificial Intelligence (AI)
Artificial intelligence and machine learning are two interconnected fields within computer science, and they play vital roles in the creation of intelligent systems. While these terms are often used interchangeably, they represent different concepts in many contexts.
What is Machine Learning (ML) in Healthcare?
Machine learning is considered a subset of artificial intelligence, defined as the ability of machines to imitate intelligent human behavior. AI systems tackle complex tasks similarly to how humans approach problem-solving.
In healthcare, machine learning serves as a powerful tool that supports medical professionals with patient care and the management of clinical data. It involves programming computers to replicate human thought processes and learning patterns.
This technology can be effectively utilized in healthcare for tasks such as gathering and managing patient information, analyzing healthcare trends, suggesting treatments, and much more. Many hospitals and healthcare organizations are beginning to appreciate how machine learning enhances decision-making and mitigates risks in medicine, leading to a surge in exciting job opportunities.
Machine learning in healthcare is a swiftly advancing field that is more accessible than it may seem. Initially intimidating, the concepts of “artificial intelligence” and “machine learning” are grounded in basic mathematical and programming principles. Once you grasp the fundamentals of machine learning, you can leverage these skills for more complex ideas and challenges, paving the way for innovation and diverse career paths.
What is Artificial Intelligence (AI) in Healthcare?
Artificial intelligence in healthcare refers to the use of machine-learning algorithms and software to simulate human cognition when analyzing, presenting, and interpreting complex medical and health data. It’s the ability of computer algorithms to draw conclusions based solely on input data.
AI technologies are becoming increasingly prevalent in both business and everyday life, and they are making their mark in healthcare as well. These advancements have the potential to assist healthcare providers in various areas of patient care and administrative tasks, enhancing existing solutions and enabling quicker resolutions to challenges. While the applications of AI and technology within healthcare are highly relevant, the strategies they support can vary widely from one hospital or organization to another. Some discussions about AI in healthcare suggest that it can match or even surpass human performance in specific tasks like disease diagnosis, but it may be some time before AI reaches its full potential in the medical field.
Key Differences Between Machine Learning (ML) and Artificial Intelligence (AI) in Healthcare
Artificial Intelligence (AI) involves intelligent computers that can think and carry out tasks autonomously, while machine learning refers to how these systems acquire intelligence. One approach to training computers to emulate human reasoning is through neural networks, which consist of a series of algorithms inspired by the human brain.
AI is often a vague term, leading to confusion between it and machine learning. Essentially, artificial intelligence describes any system that behaves intelligently, but this definition is somewhat broad, similar to saying something is “healthy.” Behaviors such as problem-solving, learning, and planning are achieved by analyzing data and recognizing patterns to replicate those actions. On the other hand, machine learning is a specific type of artificial intelligence where machines digest data to learn aspects of the world that would challenge human comprehension. Moreover, machine learning can potentially exceed human intelligence and is primarily leveraged for processing large volumes of data.
Artificial Intelligence (AI):
Artificial intelligence (AI) is the technology that allows machines to replicate human behavior.
- The objective of AI is to develop intelligent systems capable of resolving complex problems in a human-like manner.
- In AI, we design systems that can perform tasks typically carried out by humans.
- Machine learning and deep learning are two main subsets of AI.
- The applications of AI are incredibly varied.
- AI strives to create intelligent systems capable of handling numerous complex tasks.
Machine Learning (ML):
Machine learning is a subset of AI that enables machines to learn from past data without explicit programming.
- The aim of machine learning is to empower machines to learn from data and deliver accurate outputs.
- In ML, we utilize data to train machines for specific tasks to produce precise results.
- Deep learning is a key branch of machine learning.
- Machine learning has a more focused range of applications.
- Machine learning is utilized to develop machines that can carry out various tasks.
Key Advantages of Cloud Computing in Healthcare:
Cloud technology supports various healthcare innovations, including electronic medical records, mobile applications, patient portals, IoT devices, and big data analytics. Its flexibility enhances the decision-making process across the board.
Understanding Cloud Computing in Healthcare
Cloud computing in healthcare involves using remote servers, accessed through the internet, to store, manage, and process medical data. This approach differs from the traditional method of relying on on-site data centers or personal computers.
The cloud offers a scalable solution, enabling healthcare providers and facilities to store vast amounts of data securely, with management handled by IT experts.
Different Types of Cloud Computing in Healthcare:
There are four primary types of cloud computing: private clouds, public clouds, hybrid clouds, and multi-clouds.
Public Clouds:
Public clouds utilize IT infrastructure that is typically not owned by the end user. Leading providers include Alibaba Cloud, Amazon Web Services (AWS), Google Cloud, IBM Cloud, and Microsoft Azure.
Traditionally, public clouds operated on client premises, but contemporary providers also offer services on clients’ locations, blurring the lines between ownership and geographical distinction.
Private Clouds:
Private clouds are dedicated environments that serve a single user or group, often secured behind their own firewall. When the IT infrastructure is committed to one customer with exclusive access, it is defined as a private cloud.
Today, private clouds do not necessarily need to be based on on-premise infrastructure; they can also be created using rented data centers managed by vendors off-site, making location and ownership guidelines less relevant.
Managed Private Clouds:
In this setup, customers utilize a private cloud managed by a third-party vendor who handles its deployment and configuration. Managed private clouds are a viable solution for companies with limited IT staff, facilitating enhanced private cloud services and infrastructure.
Dedicated Clouds:
A dedicated cloud can be part of a public or private cloud, functioning as a separate entity within a broader cloud framework. For instance, an organization might have a dedicated cloud for its accounting department within its private cloud infrastructure.
Hybrid Clouds:
Hybrid clouds consist of a unified IT environment that integrates multiple systems connected through local area networks (LANs), wide area networks (WANs), virtual private networks (VPNs), and/or APIs.
The characteristics of hybrid clouds can be complex, with requirements varying based on differing perspectives. Some general criteria for a hybrid cloud include:
- At least one private cloud and one public cloud.
- A minimum of two private clouds.
- At least two public clouds.
- A physical or virtual environment connected to at least one public or private cloud.
Multi-Clouds:
Multi-cloud strategies involve using multiple cloud services from various vendors, whether public or private. While every hybrid cloud is inherently a multi-cloud, not every multi-cloud qualifies as a hybrid cloud. Integration or orchestration of distinct clouds creates what we term hybrid clouds.
Benefits of Cloud Computing in Healthcare
The advantages of cloud computing in healthcare extend to both patients and providers. Key benefits include lower costs, enhanced privacy, and improved patient care through better collaboration and interoperability. This alignment of business and patient outcomes is a hallmark of cloud technology in healthcare.
- Cost Reduction in Data Storage:
Setting up on-site data storage requires significant initial investments in hardware and IT infrastructure to ensure data security and accessibility.
With cloud-based healthcare solutions, providers can rely on vendors to oversee the creation and maintenance of data storage, allowing them to reduce upfront costs and concentrate on their primary mission: patient care.
- Facilitating Big Data Applications:
The shift to cloud-based data storage in healthcare has paved the way for significant “big data” initiatives aimed at improving patient outcomes.
Historically, patient records were kept on paper, leading to a wealth of untapped data in electronic medical records (EMRs) that could be crucial for predicting epidemics, unveiling correlations in patient illnesses, and determining effective treatment options.
- Enhanced Data Interoperability:
As we advance in digital health, interoperability among connected medical devices and various data systems will become increasingly critical.
With a growing number of developers creating IoT-enabled healthcare devices, the lack of standardized communication and data transfer methods hinders the benefits of an interconnected healthcare ecosystem.
- Improving Patient Safety:
Cloud computing contributes to patient safety by preventing issues like over-prescription of medications, which can be harmful. Additionally, it helps hospitals avoid unnecessary tests that patients have already undergone at other facilities, saving resources and costs.
Artificial Intelligence (AI) in Healthcare 2023: Benefits and Challenges
AI is transforming healthcare by enabling providers to analyze vast amounts of data, helping them gain insights into patient trends and needs. As technology evolves and new medical applications emerge, doctors and nurses can offer better guidance, support, and feedback to their patients.
What Does Artificial Intelligence (AI) Mean for Healthcare?
The landscape of healthcare delivery is rapidly changing due to breakthroughs in Artificial Intelligence (AI) and Machine Learning (ML). Health organizations now possess extensive data sets, including demographic information, claims data, clinical trial results, and health records. AI technologies are particularly well-suited to evaluate this data, uncovering patterns and insights that may elude human analysis. By leveraging deep learning algorithms, healthcare organizations can enhance both operational and clinical decision-making, ultimately improving patient experiences.
Benefits of Artificial Intelligence (AI) in Healthcare
In the United States, various Machine Learning (ML) technologies are available to streamline diagnostic processes. This leads to earlier disease detection, more reliable medical data analysis, and enhanced access to healthcare, particularly for underserved populations.
- Managed Concept of Health:
AI can help healthcare organizations actively identify and mitigate risks, fill gaps in preventive care, and gain a deeper understanding of how clinical, genetic, behavioral, and environmental factors affect populations. By consolidating diagnostic information, examination results, and unstructured narrative data, healthcare providers can create a comprehensive view of individual health, leading to valuable insights for disease prevention and wellness promotion. AI technologies can analyze and benchmark this data against population-level trends to spot early disease risks.
- Decision-Making in Medicine:
AI can reduce the time and resources needed to assess and diagnose patients, allowing healthcare professionals to respond more swiftly and potentially save more lives. Machine Learning algorithms are capable of identifying risks with much greater accuracy and speed compared to traditional methods. When utilized correctly, these algorithms can expedite diagnoses and lower the occurrence of diagnostic errors, a primary contributor to medical malpractice cases.
- AI-Aided Surgery:
One of the most advanced applications of AI in healthcare is the use of surgical robotics. AI-powered surgical systems can perform intricate movements flawlessly, which can reduce average procedure wait times, lower risks, minimize blood loss, and decrease complications and side effects associated with surgeries.
- Increase Effectiveness and Performance:
Today’s complex healthcare operations consist of intricately woven systems and processes. This complexity makes it challenging to minimize patient wait times, optimize resource use, and control costs.
To navigate the sea of big data in their digital environments and extract actionable insights that enhance workflow, productivity, and performance, healthcare systems are increasingly relying on AI. For instance, AI and ML can
- Boost throughput and the effective, efficient use of facilities.
- Enhance revenue cycle effectiveness by streamlining processes like prior authorization, claims, and denials.
- Automate routine tasks, allowing human resources to be allocated where they are needed most.
Challenges of Artificial Intelligence (AI) in Healthcare
One of the significant hurdles in implementing AI in healthcare is integrating it with legacy systems. These older frameworks often rely on outdated technologies, which can complicate data exchange necessary for effective AI applications.
- Understanding AI Results:
As AI models become more sophisticated, they often operate as “black boxes,” making it difficult for healthcare professionals to understand the rationale behind specific results. This lack of transparency can create challenges in trust and reliability for both healthcare organizations and patients.
- Innovative Data Annotation Techniques:
Acquiring high-quality medical data remains a significant challenge in the healthcare sector. Due to the sensitivity and ethical concerns surrounding medical data, obtaining access can be time-consuming and costly. Automated processing can still be arduous, as annotating a single model may require thousands of images.
New methods of medical image annotation are helping to address this issue by allowing for the extraction of additional datasets from individual images, significantly reducing the amount of data needed to train models.
- Invest in Privacy-Enhancing Technology:
Privacy is a critical concern in the healthcare industry. Regulations such as the General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA) safeguard sensitive Personally Identifiable Information (PII) in patient data, including medical records and identity information. The significant data requirements of most AI models, along with concerns about potential data breaches, can hinder the adoption of AI in healthcare.
- Enhance Engagement and Training for Healthcare Staff:
A primary concern for healthcare professionals regarding AI is its impact on employment. While technology will undoubtedly automate repetitive tasks and create new job roles, this can slow the adoption of AI in healthcare settings.
Although AI applications can efficiently complete specific tasks, they are far from replacing most roles in the healthcare sector. Many specialized positions require human expertise and are considerably more complex than narrowly defined tasks.
- Educate Patients to Reduce Resistance:
People tend to resist change, especially in healthcare, where familiarity is often preferred. Patient reluctance to embrace both new and familiar technologies poses a significant challenge to the implementation of AI in healthcare.
In today’s healthcare landscape, artificial intelligence is becoming increasingly prevalent, leading to transformative digital advancements. As new tools and resources emerge, many developed nations are actively adopting AI-driven technologies, particularly voice-activated and digital assistants, marking a significant shift from a physician-centered approach to a model that prioritizes patients.
Electronic Health Records (EHR) play a crucial role in converting patient information from physical files to digital formats. While EHRs have done an admirable job of securely collecting and storing patient data, they have evolved beyond just record-keeping in recent years.
In medical facilities worldwide, information technology has become essential for healthcare providers. EHRs have transitioned from simple storage solutions to comprehensive systems that facilitate data sharing among physicians, patients, and specialists. Some software offers valuable insights that support clinical decision-making by giving healthcare professionals a broader understanding of patient histories and treatment options. Overall, EHRs are positively impacting public health outcomes across the globe.
Most healthcare providers recognize that electronic data systems enhance patient care, while some also appreciate the clinical benefits these tools bring to their practices. Many medical institutions are exploring technological advancements such as data standardization, artificial intelligence, and predictive analytics to optimize EHR systems and refocus their efforts on improving patient care.
How EHRs Enhance Patient Care:
Electronic health records, once viewed merely as data entry systems, are now placing patients at the center of their care. These digital solutions boast advanced features that facilitate the analysis of patient information, enable communication among healthcare professionals, and allow for secure information sharing. Today’s EHR systems provide essential tools that help streamline operations and enhance patient outcomes. Below are some key ways EHRs have demonstrated their ability to improve patient care over time.
Improved Patient Engagement
EHR software is vital in closing the gap between patients and providers. Its integrated features assist clinics in daily operations while enhancing patient satisfaction. When visits overwhelm patients with information, they may not fully grasp what is shared. However, through patient portals, they can access important documents at their convenience. Additionally, the ability to send online prescriptions directly to their preferred pharmacies boosts patient satisfaction and adherence. When patients feel informed about their health journey, they’re more likely to follow their provider’s recommendations. Keeping them engaged throughout the process fosters compliance and a smoother experience.
Focus on Preventive Care
Electronic medical records offer robust management tools that help monitor various health conditions. They assist healthcare providers in reminding patients about check-ups and screenings. EHR systems can also identify risk factors and health habits, enhancing preventive care strategies. By receiving timely reminders for essential screenings, patients can better educate themselves and address potential health risks. Early detection of health issues can be life-saving and can help prevent complications.
Better Patient Outcomes
Clinic-based EHR systems enable administrative staff to collect, record, store, and monitor patient health information seamlessly. Healthcare providers, including doctors, nurses, and lab technicians, gain a comprehensive view of patient interactions, leading to improved outcomes. EHRs centralize patient data, allowing for the identification of health trends and better analytics that support decision-making. This results in more effective treatment plans and ultimately enhances the quality of clinical care patients receive.
Final Words
The transition from traditional medical record systems to EHRs has a significant impact on the quality of patient care delivered. With the help of SimboAI, the future of healthcare is here! From intelligent robots to e-prescriptions, SimboAI is revolutionizing the landscape of Medicare.
Exploring the Potential of Chat Generative Pre-trained Transformer 3 (GPT-3) in US Healthcare
What is Chat GPT-3?
Chat GPT-3, or Generative Pre-trained Transformer 3, is a cutting-edge natural language processing (NLP) model developed by OpenAI.
This model is capable of performing a variety of language-related tasks including translation, paraphrasing, and answering questions. Its design aims to generate text that closely resembles human writing.
Because it has been trained on a vast dataset sourced from the internet, GPT-3 can create content that is often indistinguishable from what a human might write.
Utilizing a transformer architecture, a type of neural network optimized for sequential data like language, GPT-3 can rapidly process long sequences of text, making it especially effective for tasks such as summarization and translation.
The remarkable language generation capabilities of GPT-3 have garnered significant interest due to its potential applications, though it is essential to use this technology responsibly while considering any potential drawbacks.
How Does Chat Generative Pre-trained Transformer 3 (GPT-3) Work?
In the realm of healthcare, GPT-3 could streamline administrative tasks like scheduling appointments and processing insurance claims. By automating these functions, healthcare professionals can redirect their focus towards patient care.
Unlike conventional chatbots, Chat GPT-3 does not operate online and lacks real-time access to external data sources. Instead, it generates responses based solely on the information it was trained on, which consists of a diverse range of texts from books, papers, and websites.
While the underlying technology that powers GPT-3 seems straightforward, the complexity resides in its ability to deliver quick and relevant responses to user prompts.
To train this model, a massive dataset of approximately 570GB was compiled from various sources, including books, websites, and articles, amounting to about 300 billion words.
How Medical Professionals Might Utilize GPT-3 in Healthcare?
Medical professionals, who are tasked with providing knowledgeable responses through written and verbal communication, aim to be experts in their fields. They must stay updated on the latest information regarding their specialties and related pharmaceuticals to deliver the most accurate guidance.
These professionals are often required to craft tailored responses and adjust their answers based on various inquiries, which necessitate consulting extensive medical literature.
Streamlining Administrative Tasks:
GPT-3 can help automate various administrative processes in healthcare, such as appointment scheduling and insurance claim processing.
By alleviating some of the workload, healthcare workers can focus more on providing care to patients.
Delivering Personalized Health Advice:
The model can be utilized to analyze patient data and provide tailored health suggestions, such as lifestyle changes or treatment options.
This capability may enhance treatment outcomes and overall wellness.
Enhancing Mental Health Support:
GPT-3 can also facilitate counseling or therapy sessions through conversation, offering additional mental health support.
This allows individuals to access mental health services conveniently and privately.
Challenges of Using GPT-3 in Healthcare
One of the significant challenges associated with GPT-3 is inherent bias. Like all machine learning models, its performance is only as reliable as the data it was trained on. In other words, if the training data has flaws, the model’s output can also reflect those issues.
Here are some specific challenges that GPT-3 faces in the healthcare sector:
Lack of Diversity and Bias:
The training data for GPT-3, similar to many other AI models, may exhibit biases and lack diversity. This can lead to biased outcomes and perpetuate harmful stereotypes.
Privacy and Security Concerns:
As with any AI technology that processes substantial amounts of data, there are concerns regarding data security and privacy associated with GPT-3.
Dependence on a Single Solution:
Relying solely on one AI model, such as GPT-3, can make it difficult to transition to alternative solutions if needed.
Final Thoughts on Chat GPT (Conclusion)
In summary, Chat GPT is a powerful tool for chatbots and other conversational AI applications. It combines sophisticated AI techniques like transformer architecture with extensive pre-training to generate human-like responses and engage in diverse and meaningful conversations with users. Its adaptability across different contexts allows it to provide crucial and relevant information tailored to various scenarios.
However, it is vital to acknowledge its limitations and use it judiciously. Careful selection and preprocessing of training data, awareness of potential biases, and understanding the model’s computational requirements are essential for determining appropriate applications.
By addressing these challenges and thoughtfully employing Chat GPT and similar AI models, we can maximize their benefits while minimizing any potential drawbacks.
Speech recognition and transcription are powerful tools for quickly converting spoken language, numbers, or acronyms into written text. These technologies find a wide range of applications, with some of the most prominent being in healthcare documentation, legal document preparation, and video transcription for both educational and entertainment purposes. While both methods can achieve similar outcomes in these areas, each comes with its own set of advantages and challenges. There’s also a blended approach where human editors refine speech recognition outputs for better accuracy.
What is Medical Transcription in Healthcare?
Medical transcription (MT) involves the manual conversion of voice recordings dictated by physicians and other healthcare professionals into written text. Typically, a hospital’s MT team receives audio files containing these dictations and subsequently transforms them into written medical documents.
These transcribed medical reports are usually processed digitally and submitted to the hospital’s Electronic Health Record (EHR) or Electronic Medical Record (EMR) systems.
What is Speech Recognition in Healthcare?
Medical speech recognition (MSR) refers to any technology that allows users to speak instead of type. This technology transcribes spoken words directly onto the screen.
Healthcare professionals, such as doctors and nurses, can use voice recognition software to take notes on their laptops without interrupting patient care. This ability lets them complete their work more efficiently, allowing more time for patient interactions and other essential activities.
About Transcription in Healthcare
Medical transcriptionists employ digital equipment to convert audio recordings from healthcare professionals into formal reports. They are often referred to as healthcare documentation specialists, and they may further edit these medical records for accuracy before they are submitted for review and approval.
Types of Transcription –
Dictation for Medical Reports:
Dictating reports is one of the most familiar forms of medical transcription. Picture this: you visit a physician who evaluates your symptoms and offers recommendations. Just before you leave, they pull out a recording device to narrate the details of your visit. Later, this information is transcribed by their receptionist or a specialized transcriptionist into a medical report. This document could either be filed for future reference during your next visit or sent to another specialist.
Medical Interview Transcription Services:
Healthcare professionals often hold regular consultations and interviews. These sessions may cover recent advancements in the medical field, regulatory changes, updates from medical charities, or discussions about clinical treatment recommendations and the welfare of staff and practitioners. Such medical interviews are usually recorded by trained professionals using digital recorders or smartphones, which can sometimes result in poor audio quality. Therefore, it’s imperative for our medical transcriptionists to possess a keen ear for clarity amid background noise.
Pros of Transcription –
The benefits of medical transcription services for healthcare providers ensure that patients receive accurate diagnoses, treatments, and prescriptions. Especially when compared to using speech recognition software alone, these services help minimize errors and enhance the precision of medical records.
Cons of Transcription –
While medical dictation software has simplified tasks for both patients and healthcare providers, some drawbacks can hinder its convenience.
Today’s transcription services are heavily reliant on technology, and even minor technical issues can significantly disrupt the process. Faulty data drives, software glitches, and communication problems can severely affect functionality.
Additionally, transcripts may not always be updated to reflect changing regulations at local, state, or federal levels, highlighting the necessity for ongoing documentation and transparency for compliance purposes.
About Speech Recognition in Healthcare
Medical speech recognition (MSR) refers to technologies that enable individuals to speak rather than type. This spoken dictation is directly transcribed onto a digital panel.
Types of Speech Recognition –
Back-end:
These systems convert speech to text only after the speaker has finished their dictation. The audio file is recorded, transcribed, and then transformed into a written document for review and use.
Front-end:
In contrast to back-end systems, Front-end Speech Recognition (SR) systems transcribe speech to text in real-time. A medical professional must modify the text to correct any mistakes made by the system or to help the software understand their specific phrasing better.
Speaker-dependent:
This type of software recognizes the unique features of an individual’s voice, requiring new users to speak to the system to help it learn how to function properly.
Speaker-independent:
Devices in this category can comprehend any user’s speech without prior training. However, the trade-off is lower accuracy compared to speaker-dependent systems, as they often operate with a limited vocabulary and syntax to manage complexity.
Control Panel:
SR systems equipped with a control interface allow users to interact with various software through voice commands. In healthcare, such systems facilitate data entry across different Electronic Medical Record (EMR) fields, assist with ordering and inventory management, and support other administrative tasks.
Pros of Speech Recognition –
Utilizing an EHR system with voice recognition reduces errors due to fewer clicks and expedites the documentation process. Physicians can seamlessly create, document, edit, and verify digital records.
This is particularly beneficial since many healthcare professionals struggle to find time for their documentation. Thanks to speech recognition technology, clinicians can swiftly record their notes, capturing vital information about diagnoses, medications, and treatments efficiently, ultimately saving time and making interactions with patients more manageable.
Cons of Speech Recognition –
A significant challenge with speech recognition is data recall. You might not capture every detail from your patient interactions when using this voice transcription method.
Furthermore, implementing voice recognition technology can be costly, often requiring specialized software and hardware for optimal performance. Additionally, practitioners may need extensive training to utilize these voice recognition systems effectively.
BENEFITS OF MEDICAL TRANSCRIPTION
Medical transcription services offer numerous benefits for healthcare providers, ensuring that patients receive the right treatments and medications. When compared to relying solely on voice recognition software, these services significantly lower error rates and enhance the accuracy of records.
What is Medical Transcription?
Medical transcription involves converting voice recordings made by healthcare professionals such as doctors or nurses into written text. A trained professional, equipped with medical knowledge and a grasp of language intricacies, listens to these recordings and produces medical transcripts. This process includes transcribing various documents such as lab reports, patient charts, medical histories, physician reports, emergency room notes, surgical summaries, discharge summaries, rehabilitation reports, and more.
Benefits for Healthcare Providers, Hospitals, and Practices
Medical transcription services are essential for numerous healthcare organizations, including:
- Hospitals
- Physician’s offices
- Medical organizations
- Insurance companies
- Government agencies
- Other healthcare-related industries
Numerous physicians nationwide depend on professional medical transcriptionists to ensure that patient records are accurately documented and readily available at the time of care. This service becomes particularly vital for doctors handling rare cases or those practicing in rural areas where qualified personnel may be scarce.
By utilizing transcription services, healthcare providers such as physicians, nurse practitioners, and physician assistants can focus more on providing care to patients, confident that their reports will be accurately documented in a timely manner and accessible when needed.
Effective medical transcription services streamline the documentation process, allowing healthcare professionals to dedicate more time to patient care while minimizing the risk of errors that can arise from handwritten reports. Accurate documentation has been shown to enhance reimbursement rates and reduce liability risks; these benefits are often reflected in higher reimbursements from third-party payers and lower premiums for personal injury coverage from insurance companies.
Benefits of Medical Transcription:
Medical transcription is the process of translating spoken words from a healthcare provider into text, which can be stored electronically or as a physical document in a patient’s file. This system provides numerous advantages for medical practices, outlined below:
1. Efficient Time Management:
In a busy healthcare environment, it’s easy to become overwhelmed. Patients can be referred at any hour, schedules vary dramatically, and keeping everything organized is crucial for the smooth operation of your office.
2. Enhanced Quality of Care:
With well-organized information, you can access your patient’s complete history easily, including past conversations. Reviewing prior notes can jog your memory on key details of a case, leading to improved patient care.
3. Versatile Information Sources:
You don’t need an expensive recording device to benefit from medical transcription. In fact, many smartphone apps are just as effective as traditional dictation tools. The portability of these devices allows you to capture not only your insights but also your patient’s input, which can be beneficial for complex cases.
4. Cost Reduction:
Saving time translates to saving money, but the benefits of medical dictation and transcription extend beyond that. By using transcription software to organize information, you can reduce the costs associated with acquiring necessary data, streamline billing, and enhance overall efficiency.
5. The EMDAT System:
EMDAT (Electronic Medical Dictation and Transcription) addresses the challenges of documenting patient care information effectively.
- Manages and routes documentation efficiently
- Compiles essential information
- Supports various input and recording devices
- No need to use a computer while interacting with patients
- Lowers transcription costs
- Boosts productivity and profitability
6. High-Quality Medical Records:
With strict adherence to HIPAA regulations, medical transcription services are essential for ensuring the accuracy and confidentiality of patient records. All documentation must undergo rigorous multi-level quality assurance processes, which encompass formatting, copy editing, and thorough review.
How Simbo.AI Enhances Medical Transcription:
Simbo is committed to simplifying data gathering and documentation between healthcare providers and patients.
Simbo has developed cutting-edge technology that acts as an AI-Powered Medical Scribe. Our AI-driven voice recognition software allows providers to converse naturally while generating clinically accurate notes, complete with relevant structured data. Simbo not only comprehends medical terminology but also grasps context, enabling providers to communicate freely without the need to adjust to complicated software.
Our voice-enabled AI streamlines the workflow for patients, administrative staff, clinical teams, and, most importantly, the providers. This solution facilitates easy documentation, enhances patient engagement, reduces the burden of electronic medical records (EMRs), and could potentially save providers up to three hours each day. Simbo helps combat burnout, increases productivity, and fosters more engaged and satisfied patients.
Simbo.AI harnesses a human-like intelligence to address the evolving needs of healthcare. It’s designed to listen to both doctors and patients, ensuring real-time, digital documentation of medical records.
Additionally, Simbo.AI can transform voice recordings from physicians and other healthcare professionals into formal reports. A human review team can optionally edit these transcribed records for accuracy before they are finalized for review and approval.